For decades, marijuana withdrawal was dismissed—by doctors, by society, and by users themselves. "Weed isn’t addictive" became the default assumption. But the science tells a different story. Cannabis Withdrawal Syndrome (CWS) was added to the DSM-5 in 2013, and research since then has only strengthened the case: marijuana withdrawal is real, physiologically driven, and experienced by roughly 47% of regular users who stop.
If you’re going through it right now, this guide covers everything the research says about what’s happening in your body, what symptoms to expect, how long they last, and what actually helps.
Is Marijuana Withdrawal Real?
Yes. Unambiguously.
Cannabis Withdrawal Syndrome is a recognized clinical diagnosis in both the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders) and the ICD-10 (International Classification of Diseases). Diagnosis requires at least three of the following symptoms developing within a week of cessation after heavy, prolonged use:
- Irritability, anger, or aggression
- Nervousness or anxiety
- Sleep difficulty (insomnia, vivid dreams)
- Decreased appetite or weight loss
- Restlessness
- Depressed mood
- Physical symptoms: abdominal pain, shakiness, sweating, fever, chills, headache
A meta-analysis published in Substance Abuse and Rehabilitation found that approximately 47% of frequent cannabis users experience clinically significant withdrawal. That number rises to over 50% for daily users. Among people seeking treatment for cannabis use disorder, withdrawal rates exceed 80%.
The reason marijuana withdrawal was dismissed for so long is partly because it is less dramatic than alcohol or opioid withdrawal. There is no risk of seizures or death. But "less dangerous" does not mean "not real." The symptoms are genuine, neurologically driven, and for many people, severe enough to drive relapse.
Why Marijuana Withdrawal Happens
Withdrawal happens because regular THC exposure fundamentally changes your brain’s chemistry. Two systems are primarily affected:
The Endocannabinoid System
Your brain has its own cannabinoid system—the endocannabinoid system (ECS). It produces natural compounds (anandamide and 2-AG) that regulate mood, sleep, appetite, pain perception, and stress response through CB1 and CB2 receptors.
THC is structurally similar to anandamide and binds to the same CB1 receptors—but at much higher concentrations. With regular use, your brain adapts by reducing the number of CB1 receptors (downregulation) and producing less anandamide. The system recalibrates around the assumption that THC will always be present.
When you stop, your brain has fewer receptors and less natural cannabinoid production. The functions that the ECS regulates—sleep, appetite, mood, temperature—all become dysregulated. This is the direct cause of most withdrawal symptoms.
Research from Molecular Psychiatry shows that CB1 receptor density begins recovering within 2 days of cessation, with significant recovery by day 28 and near-complete normalization by day 90. This neurological timeline is why the 90-day recovery framework exists.
The Dopamine System
THC triggers dopamine release in the nucleus accumbens—your brain’s reward center. With chronic use, the brain reduces baseline dopamine production and receptor sensitivity. When THC is removed, dopamine levels drop below normal.
This is why everything feels flat, grey, and joyless during the first weeks of quitting. It is not depression in the clinical sense (though it can feel identical). It is a temporary neurochemical deficit that resolves as dopamine systems normalize—typically over 4–12 weeks.
Marijuana Withdrawal Symptoms
Klar tracks 47 documented withdrawal symptoms. Below are the most common, grouped by category. Each links to a detailed guide with neuroscience explanations, expected timelines, and coping strategies.
Sleep Symptoms
- Insomnia — Reported by 46–71% of people quitting. Often the most disruptive symptom. Caused by the loss of THC’s sedative effect and ECS dysregulation of sleep-wake cycles.
- Vivid dreams and nightmares — REM rebound after THC suppression. Dreams become unusually intense, vivid, and sometimes disturbing. Peaks around days 3–7.
- Night sweats — Thermoregulation disruption as the ECS recalibrates. Your body loses its artificial temperature regulation.
Psychological Symptoms
- Anxiety — Reported by 50–76% of people. Caused by GABA/glutamate imbalance and loss of THC’s anxiolytic effect. Peaks days 3–10.
- Depression — Directly tied to dopamine depletion. Flat affect, loss of interest, difficulty feeling pleasure. Usually improves significantly by week 4–6.
- Irritability and anger — Often the earliest symptom. Caused by amygdala hyperactivity without THC’s dampening effect.
- Mood swings — Emotional dysregulation as the ECS and serotonin systems rebalance.
Cognitive Symptoms
- Brain fog — Difficulty concentrating, poor memory, feeling “stupid.” Caused by prefrontal cortex recalibration. Typically resolves by weeks 2–4.
- Cravings — Reported by 75–80% of people. Driven by conditioned dopamine pathways. Peaks during week 1, then gradually weakens over 30–60 days. Craving surfing is the most effective evidence-based technique.
Physical Symptoms
- Loss of appetite — THC stimulates appetite through CB1 receptors in the hypothalamus. Without it, hunger signals are suppressed. Usually normalizes within 1–2 weeks.
- Headaches — Common in the first week. Related to changes in blood flow and neurotransmitter shifts.
- Nausea — Gastrointestinal disruption as the ECS in the gut recalibrates. Typically mild and resolves within days.
For the complete list of all withdrawal symptoms with individual guides, see our Cannabis Withdrawal Symptoms directory.
The Marijuana Withdrawal Timeline
Everyone’s experience is different, but research reveals a consistent pattern. Here is what the science shows for the average recovery trajectory:
Days 1–2: Onset
THC is still in your system. Symptoms are mild—mostly cravings, mild anxiety, and restlessness. Your brain is registering the change but full withdrawal has not begun. This is the psychological phase: habit circuits fire at every trigger.
Days 3–7: Peak Acute Withdrawal
This is the hardest stretch. Insomnia peaks. Irritability spikes. Appetite drops. Night sweats begin. Vivid dreams disrupt whatever sleep you manage to get. Cravings are at their strongest. CB1 receptors are at their lowest density. The good news: it gets better from here.
Days 7–14: Gradual Improvement
Physical symptoms begin easing. Appetite starts returning. Sleep is still disrupted but improving. Brain fog lifts partially. Cravings become less constant, though still triggered by situational cues. CB1 receptors are recovering measurably—research shows significant upregulation by day 14.
Days 14–30: Stabilization
Most physical symptoms have resolved. Sleep quality improves substantially. The challenge shifts from physical withdrawal to psychological: boredom, habit loops, and the “Valley of Disappointment” begins. Life feels better than week 1 but not as good as you expected. Dopamine systems are still normalizing.
Days 30–60: The Valley
Acute withdrawal is over, but you may not feel “great” yet. This is the period where many people relapse—not because symptoms are severe, but because the absence of dramatic improvement is demoralizing. Understanding that this is a normal neurological phase (dopamine normalization is still in progress) is critical for persistence.
Days 60–90: Recovery
Most people report feeling significantly better. CB1 receptor density has reached near-normal levels. Dopamine regulation has substantially recovered. Sleep architecture has normalized. Cravings are infrequent and manageable. You start feeling like yourself again—or like a new, clearer version of yourself.
For day-by-day breakdowns, see our complete 90-day recovery timeline.
Who Gets It Worse?
Withdrawal severity varies based on several factors identified in research:
- Duration of use: Longer use means greater neuroadaptation and potentially longer recovery.
- Frequency: Daily users experience more severe withdrawal than occasional users.
- THC concentration: Modern cannabis products (concentrates, high-THC strains) cause greater receptor downregulation than lower-potency cannabis.
- Co-occurring conditions: People with anxiety disorders, depression, or ADHD often report more severe psychological withdrawal symptoms.
- Cold turkey vs. tapering: Abrupt cessation typically produces more intense but shorter withdrawal than gradual reduction.
- Age of onset: People who started using cannabis in adolescence may experience more pronounced withdrawal, as their ECS developed in the presence of THC.
There is no way to eliminate withdrawal entirely, but understanding your risk factors helps set realistic expectations.
What Actually Helps
Based on the evidence, these are the most effective strategies:
1. Know Your Timeline
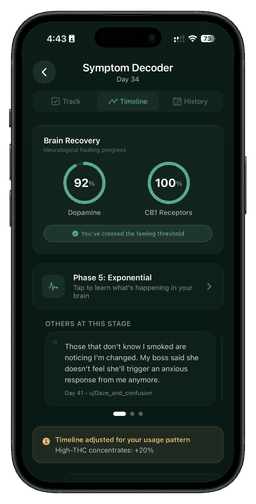
Uncertainty makes withdrawal worse. When you know that insomnia peaks around day 5 and improves by day 14, you can endure it. When you know the Valley of Disappointment is a predictable neurological phase (not a sign that you will feel flat forever), you can persist through it. Klar’s brain recovery visualization gives you this map.
2. Track Your Symptoms
Self-monitoring activates the prefrontal cortex, which counteracts the amygdala’s panic response. Tracking transforms “I feel terrible” into “Day 6: insomnia 7/10, anxiety 5/10—both expected to decrease this week.” This is not a placebo. Research on self-monitoring in substance use recovery shows measurably better outcomes.
3. Exercise
The single most effective non-pharmacological intervention for withdrawal symptoms. Exercise increases endocannabinoid production (your natural version of what THC provides), boosts dopamine, improves sleep quality, and reduces anxiety. Even 30 minutes of moderate exercise significantly reduces craving intensity.
4. Craving Surfing
The average craving lasts 15–20 minutes. Craving surfing—observing the urge without acting on it—weakens the neural pathway each time. It is derived from Mindfulness-Based Relapse Prevention, which has strong evidence for reducing substance use relapse.
5. Sleep Hygiene
Since insomnia is the most disruptive symptom, prioritizing sleep hygiene is essential: consistent sleep/wake times, cool room, no screens before bed, no caffeine after noon. Melatonin (0.5–3mg) may help with initial onset but consult a healthcare provider.
6. Social Support
Tell someone you’re quitting. Communities like r/leaves (400K+ members) provide peer support from people who understand exactly what you’re going through. Accountability and shared experience are protective factors against relapse.
When to Seek Professional Help
Most marijuana withdrawal resolves on its own within 2–4 weeks for physical symptoms and 4–12 weeks for psychological symptoms. However, seek professional help if:
- Depression is severe or includes suicidal thoughts
- Anxiety is debilitating and preventing normal functioning
- You are unable to stop using despite wanting to
- Withdrawal symptoms persist beyond 8 weeks with no improvement
- You have a co-occurring mental health condition that is worsening
Resources:
- SAMHSA Helpline: 1-800-662-4357 (free, confidential, 24/7)
- 988 Suicide & Crisis Lifeline: Call or text 988
- Crisis Text Line: Text HOME to 741741
- r/leaves: Peer support community for quitting cannabis
Frequently Asked Questions
How long does marijuana withdrawal last?
Acute physical symptoms (insomnia, appetite loss, irritability) typically last 1–3 weeks. Psychological symptoms (cravings, mood changes, anhedonia) can persist for 4–12 weeks. Full neurological recovery (CB1 receptor normalization, dopamine regulation) takes approximately 90 days based on neuroimaging research.
Can you die from marijuana withdrawal?
No. Unlike alcohol or benzodiazepine withdrawal, cannabis withdrawal does not produce seizures or life-threatening complications. It is uncomfortable and can be psychologically distressing, but it is not medically dangerous.
Is marijuana withdrawal as bad as alcohol withdrawal?
They are different. Alcohol withdrawal is more physically dangerous (risk of seizures, delirium tremens). Marijuana withdrawal is less acute but can be more prolonged, with psychological symptoms lasting weeks to months. Neither should be dismissed.
Does CBD help with marijuana withdrawal?
Preliminary research is promising but inconclusive. Some studies suggest CBD may reduce anxiety and cravings during cannabis cessation, but the evidence is not yet strong enough for clinical recommendations. If you try CBD, ensure it contains no THC.
Is it better to quit cold turkey or taper?
Both approaches work. Cold turkey produces more intense but shorter withdrawal. Tapering (gradually reducing use over 1–2 weeks) produces milder symptoms but extends the timeline. Choose the approach you can sustain. For heavy daily users, a short taper may reduce peak symptom severity.
Marijuana withdrawal is a temporary neurological process. Your brain adapted to THC, and now it is adapting back. It is not pleasant, but it is finite, it is well-documented, and you do not have to navigate it alone. Tools like Klar and communities like r/leaves exist because millions of people have walked this path before you—and made it through.