Depression After Quitting Weed
Low mood, emotional flatness, and loss of motivation after quitting cannabis are driven by temporary dopamine system disruption and take time to resolve.
30-45% of people quitting cannabis
Day 10
~Day 45
Recovery Timeline
| Metric | Value |
|---|---|
| Prevalence among quitters | 30-45% of people quitting cannabis |
| Typical onset | Day 3 |
| Peak intensity | Day 10 |
| Expected resolution | ~Day 45 |
| Total duration | 42 days (approximate) |
Everything feels gray. Things that used to excite you feel pointless. You’re not exactly sad — it’s more like you can’t feel anything at all. If you recently quit cannabis, this emotional flatness is a well-understood neurological response, and it’s one of the clearest signs that your brain is in the process of rewiring itself.
Why Quitting Weed Causes Depression
THC triggers dopamine release in the brain’s reward circuit (the mesolimbic pathway). This is the same system activated by food, sex, social connection, and achievement. Regular cannabis use floods this system with dopamine, and your brain responds by:
- Reducing dopamine receptor density. Fewer D2 receptors means less sensitivity to dopamine signals.
- Reducing baseline dopamine production. Why make your own when THC is providing it?
- Blunting natural reward responses. Activities that should feel rewarding (exercise, socializing, completing tasks) produce a muted dopamine response.
When you quit, you’re left with a reward system that’s underproducing dopamine and undersensitive to what it does produce. The world feels flat because your brain literally can’t generate the same reward signals it could before heavy use. This is the dopamine connection — and understanding it is key to not giving up during recovery.
Researchers call this anhedonia — the inability to feel pleasure. It’s not sadness in the traditional sense; it’s the absence of emotional color. It’s the most common reason people relapse during weeks 4–6, a period we call the Valley of Disappointment.
When Does It Start, Peak, and End?
- Onset: Days 3–7. Often masked initially by the more acute symptoms (insomnia, anxiety, cravings).
- Peak: Days 10–21. As physical symptoms ease, the emotional flatness becomes more noticeable.
- The Valley: Weeks 4–6. This is the danger zone. Physical withdrawal is over, but your brain hasn’t fully recalibrated. You feel “worse” than week 1 because you expected to feel better by now.
- Recovery: Days 45–90. Dopamine receptor density and sensitivity gradually restore. Colors start coming back.
What Actually Helps
1. Understand the Valley
Knowing about the Valley of Disappointment before you hit it is protective. Weeks 4–6 are hard not because you’re getting worse but because your expectations have outpaced your brain’s recovery timeline. This is normal. It passes.
2. Stack Small Dopamine Wins
Your dopamine system needs retraining. Give it small, natural rewards throughout the day: complete a task (check it off a physical list), exercise, take a cold shower, cook a meal, talk to someone. Each one generates a small dopamine pulse that helps upregulate receptors over time.
3. Sunlight and Movement
Morning sunlight (10–15 minutes) and physical movement are the two most evidence-backed natural antidepressants. Together, they boost serotonin, dopamine, and BDNF (brain-derived neurotrophic factor, which supports neural recovery). Make them non-negotiable daily habits.
4. Social Connection (Even When You Don’t Want It)
Depression tells you to isolate. Resist this. Even a 10-minute phone call or a walk with someone activates your social reward system. You don’t need to feel like socializing for it to work neurologically.
5. Track Your Recovery
Depression distorts perception. You think nothing is improving when it actually is. Tracking your symptoms daily (in Klar or a journal) gives you objective evidence of progress that your depressed brain can’t dismiss.
When to Seek Professional Help
- Suicidal thoughts or self-harm urges — seek help immediately
- Depression is worsening (not improving) after 6 weeks
- You had depression before cannabis use (withdrawal may have unmasked a pre-existing condition)
- You cannot perform basic daily functions (eating, hygiene, work)
988 Suicide & Crisis Lifeline: Call or text 988
Crisis Text Line: Text HOME to 741741
SAMHSA National Helpline: 1-800-662-4357 (free, confidential, 24/7)
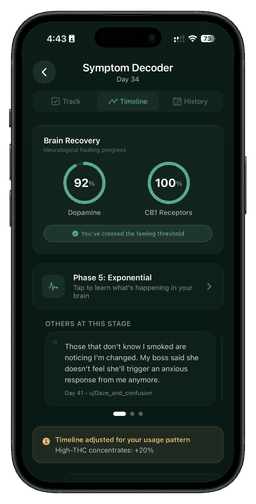
Track your progress
See your brain healing in real time
Klar tracks 47 withdrawal symptoms and visualizes your dopamine and CB1 receptor recovery day by day.
Related Symptoms
Medical Disclaimer: This content is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider with questions about a medical condition. If you are in crisis, call 988 (Suicide & Crisis Lifeline) or text HOME to 741741.