"It's just weed." "Weed isn't addictive." "You can't get hooked on marijuana." You have heard these claims. Maybe you have made them yourself. But if you are reading this, something does not feel right. Maybe you have tried to cut back and could not. Maybe your use has escalated. Maybe you are starting to wonder if "just weed" is controlling more of your life than you want to admit.
Is Weed Actually Addictive?
Yes. Cannabis can cause physical dependency and addiction, and this is not controversial in the scientific community. The condition is called Cannabis Use Disorder (CUD) and is recognized by the DSM-5, the diagnostic manual used by psychiatrists and psychologists worldwide.
Research published in JAMA Psychiatry found that approximately 30% of people who use cannabis develop some degree of cannabis use disorder. Among daily users, the rate is significantly higher.
The confusion about whether weed is addictive comes from comparing it to substances with severe physical withdrawal (alcohol, opioids, benzodiazepines). Cannabis withdrawal is real but rarely dangerous — it will not cause seizures or require medical detox. But "not as bad as heroin withdrawal" is a low bar that says nothing about whether cannabis dependency is real or harmful.
The DSM-5 Criteria for Cannabis Use Disorder
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) defines cannabis use disorder using 11 criteria. Meeting 2 or more within a 12-month period qualifies for a diagnosis:
- Using more than intended. You set out to have one joint and end up smoking three. You plan to use only on weekends but find yourself using on weekdays too.
- Difficulty cutting down or stopping. You have tried to reduce or quit and were unable to maintain it.
- Spending excessive time obtaining, using, or recovering from cannabis. A significant portion of your day revolves around weed.
- Cravings. Strong urges or desires to use cannabis, especially in triggering situations.
- Failing to fulfill major obligations. Cannabis use affecting your performance at work, school, or home.
- Continued use despite social problems. Using despite arguments with partners, friends, or family about your use.
- Giving up activities. Reducing or abandoning hobbies, social activities, or exercise because of cannabis use.
- Using in physically hazardous situations. Driving while high, operating machinery, or other risky behavior.
- Continued use despite physical or psychological problems. Knowing cannabis is contributing to anxiety, depression, lung issues, or other problems but using anyway.
- Tolerance. Needing more cannabis to achieve the same effect, or the same amount producing less effect.
- Withdrawal. Experiencing physical or psychological symptoms when you stop using: insomnia, irritability, decreased appetite, anxiety, cravings, or restlessness.
Self-Assessment: 9 Signs to Look For
Beyond the clinical criteria, here are practical signs that your relationship with cannabis may have become problematic:
1. You use cannabis to cope, not to enjoy
There is a difference between choosing to use and feeling like you need to use. If cannabis has shifted from something you do for fun to something you do to manage stress, sleep, anxiety, or boredom, that is a dependency signal.
2. Your tolerance has increased significantly
If you started with a few hits and now need a full joint, concentrate, or multiple sessions to feel the same effect, your CB1 receptors have downregulated. This is the neurological definition of tolerance and a hallmark of dependency.
3. You get irritable, anxious, or cannot sleep without it
If stopping for even one day causes irritability, anxiety, or sleep problems, you are experiencing withdrawal. Your body has adapted to the presence of THC and cannot regulate normally without it.
4. You have tried to quit or cut back and failed
This is the most honest signal. If you have told yourself "I'll only smoke on weekends" and could not stick to it, or tried to quit and relapsed within days, the pattern speaks for itself.
5. Cannabis is the first thing you think about in the morning
Whether it is looking forward to your evening session or reaching for a vape before you are fully awake, when cannabis occupies your mental space before your day even starts, it has become central to your routine in a way that goes beyond casual use.
6. You use alone more than with others
Social use can be recreational. Solitary use, especially daily solitary use, tends to indicate self-medication or dependency rather than social enjoyment.
7. You have lost interest in things you used to enjoy
This is one of the most insidious signs. When your dopamine system adapts to cannabis, other activities feel less rewarding. Hobbies, exercise, socializing, and creative pursuits gradually feel "boring" compared to getting high. This is anhedonia driven by dopamine dysregulation.
8. People in your life have expressed concern
If a partner, friend, family member, or colleague has mentioned your cannabis use, they are seeing something you may be minimizing. External observations are valuable data.
9. You are reading this article
People who do not have a problem with cannabis do not search for "am I addicted to weed." The fact that you are here suggests a part of you already knows the answer.
Mild, Moderate, or Severe?
The DSM-5 classifies cannabis use disorder by severity based on how many of the 11 criteria you meet:
| Criteria Met | Severity | Description |
|---|---|---|
| 2–3 | Mild | Early-stage dependency. Easier to address. May respond well to self-directed change with tools like Klar. |
| 4–5 | Moderate | Established dependency. Self-directed recovery is possible but may benefit from professional support. |
| 6+ | Severe | Significant dependency affecting multiple life areas. Professional support recommended alongside any self-directed tools. |
Severity is not a moral judgment. It is a clinical measure that helps determine what level of support you need. Mild CUD does not mean your struggle is not real.
Why This Is Not About Willpower
Cannabis dependency is a neurological adaptation, not a character flaw. When you use cannabis regularly, your brain physically changes: CB1 receptors downregulate, dopamine baseline drops, and your stress-response system recalibrates around the presence of THC.
Telling someone with cannabis use disorder to "just quit" is like telling someone with glasses to "just see better." The hardware has changed. Recovery requires understanding these changes and working with them, not against them.
This is why evidence-based approaches that address the neuroscience — understanding your recovery timeline, surfing cravings rather than fighting them, rebuilding your dopamine system through alternative activities — work better than willpower alone.
What to Do If You Think You Have a Problem
1. Be honest with yourself
Denial is the first barrier. If you have read this far and see yourself in multiple signs above, acknowledging it is not weakness — it is the prerequisite for change.
2. Understand what quitting involves
Knowledge reduces fear. Read about the withdrawal process, the common symptoms, and the recovery timeline. Knowing that insomnia peaks around day 5 and that the Valley of Disappointment is temporary makes these experiences manageable rather than terrifying.
3. Get the right tools
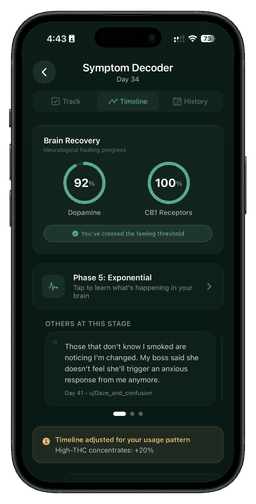
Klar was built specifically for cannabis recovery. It tracks 47 withdrawal symptoms, visualizes your brain recovery, and uses evidence-based craving management tools. Having data on your recovery makes the process less abstract and more actionable.
4. Consider professional support
For moderate to severe CUD, a therapist specializing in substance use can provide structured support. Cognitive Behavioral Therapy (CBT) and Motivational Enhancement Therapy (MET) have the strongest evidence base for cannabis use disorder.
5. Tell someone
Recovery in isolation is harder. Whether it is a trusted friend, family member, therapist, or online community like r/leaves, having even one person who knows what you are going through makes a meaningful difference.
If you are in crisis: Contact the SAMHSA helpline at 1-800-662-4357 (free, confidential, 24/7) or text HOME to 741741 for the Crisis Text Line.
Frequently Asked Questions
Can you be addicted to weed if you only smoke at night?
Yes. Frequency pattern matters less than whether you can comfortably stop. If skipping your nightly session causes sleep problems, irritability, or anxiety, you have physical dependency regardless of when you use.
Is cannabis use disorder the same as being an addict?
Cannabis use disorder is a clinical diagnosis on a spectrum (mild, moderate, severe). The word "addict" carries stigma that the clinical framework avoids. What matters is whether your cannabis use is causing problems in your life, not what label you use.
Can you be physically dependent but not addicted?
Yes. Physical dependence (tolerance + withdrawal) is one component of addiction. You can have physical dependence without the compulsive use patterns that characterize the full disorder. However, physical dependence often progresses to broader dependency over time.
How common is cannabis addiction?
Approximately 10% of all cannabis users and 30% of current users develop some form of cannabis use disorder. Among daily users, the rate is even higher. It is far more common than the "weed is not addictive" narrative suggests.